“You have severe heart damage, Mr. Patterson.”
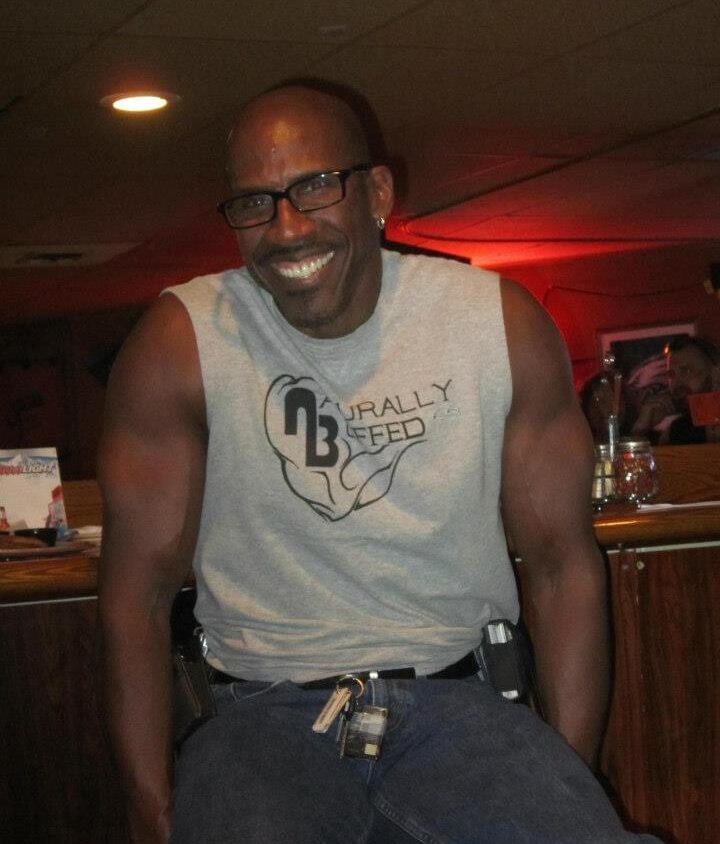
Those words literally knocked me back for a few seconds. Heart damage? ME? I mean, I’m no Jack LaLanne but I’ve maintained my weight, look, and health for close to 40 years! How’d I end up with heart damage was beyond my comprehension initially? How did this happen? WHEN did this happen? Keep reading to follow my 4-5 week heart issue journey.
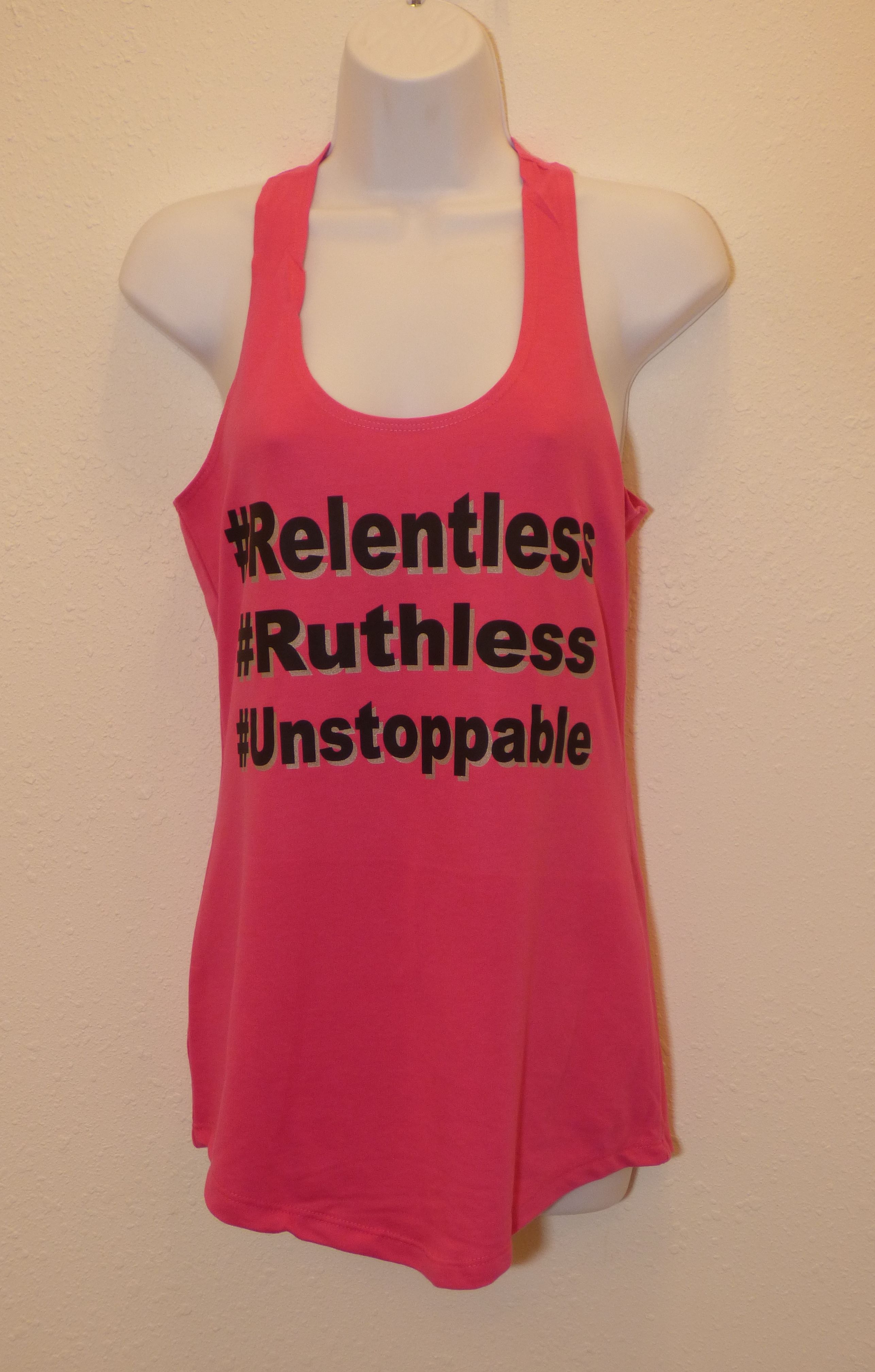
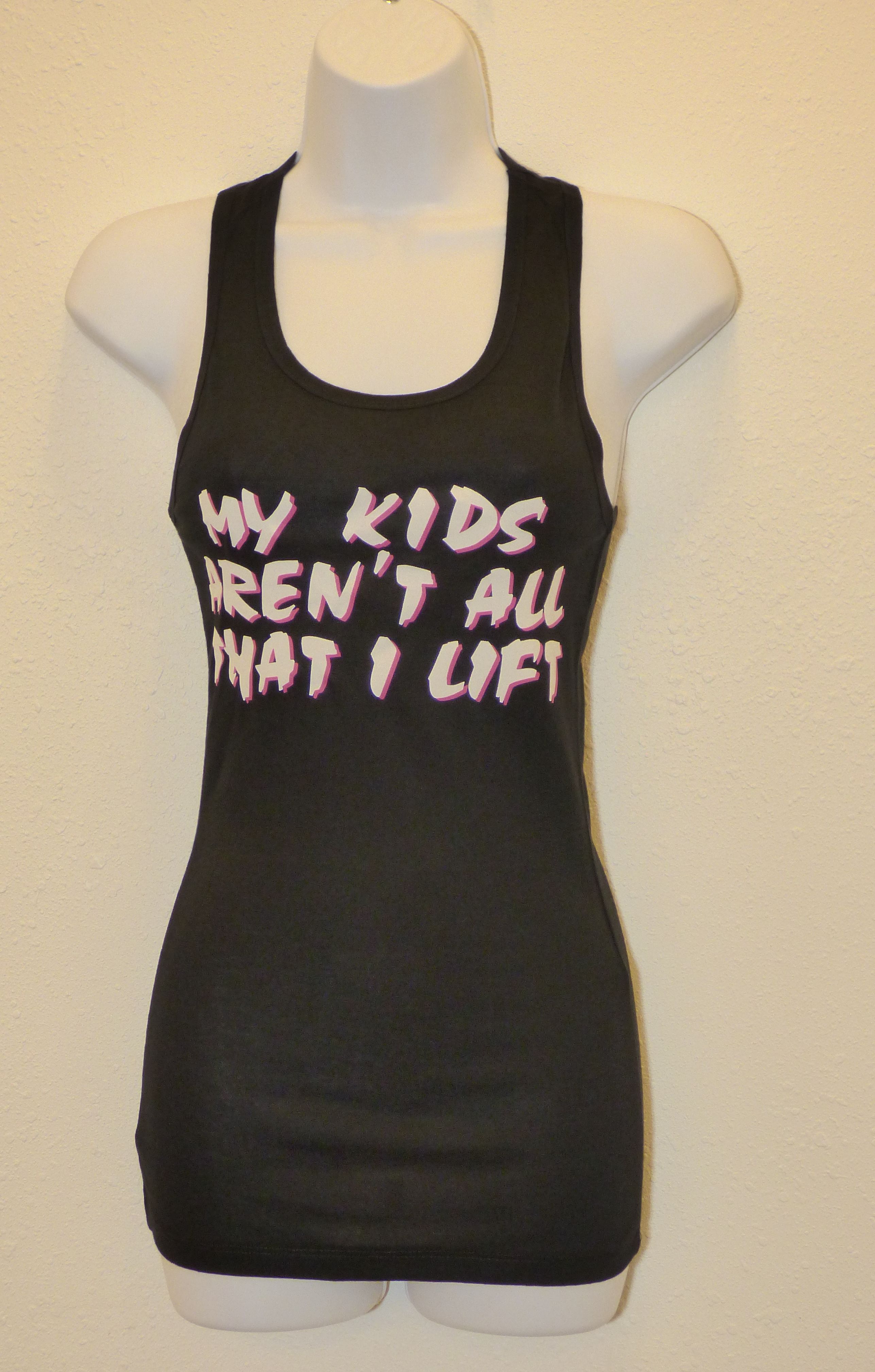
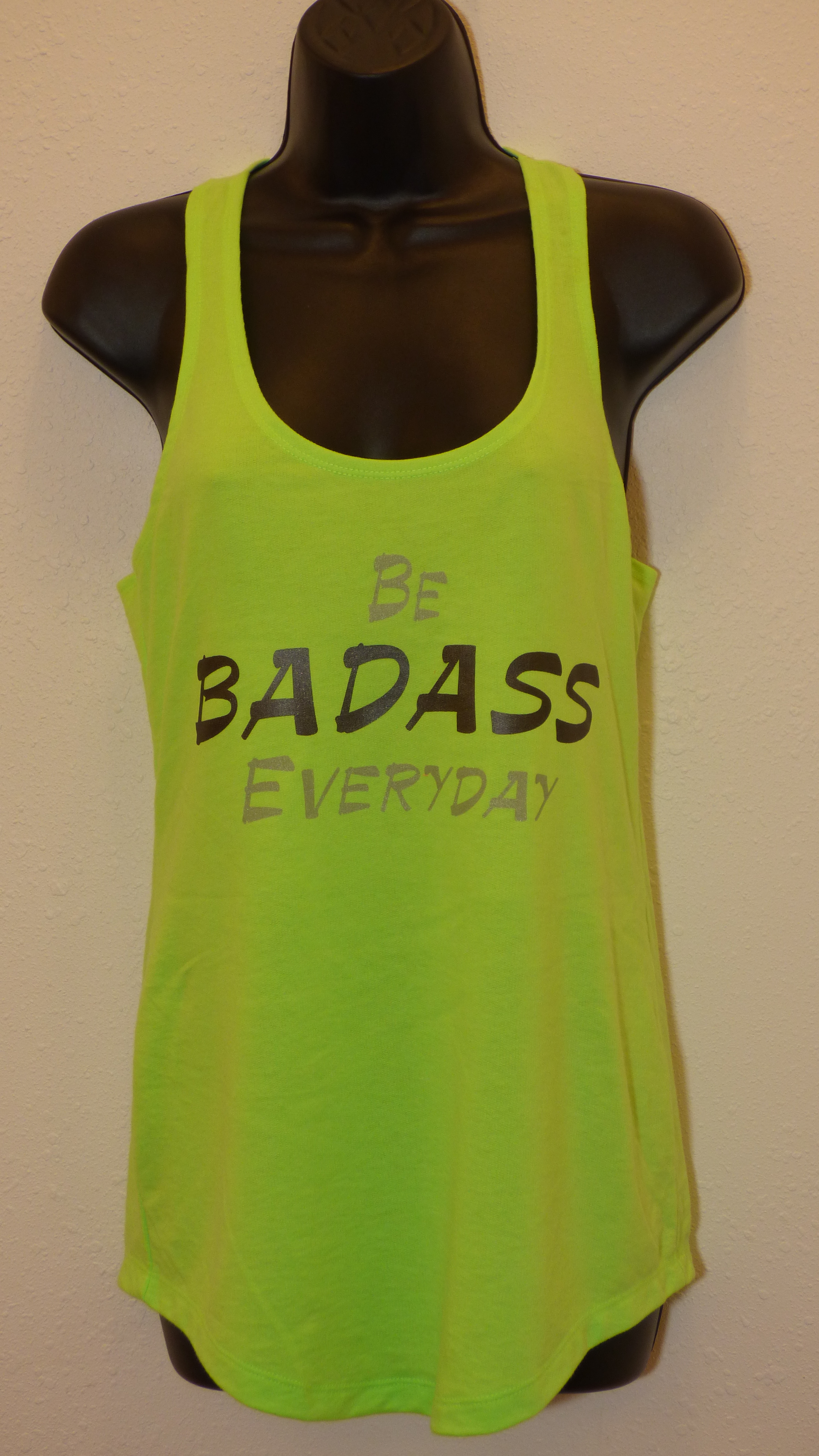
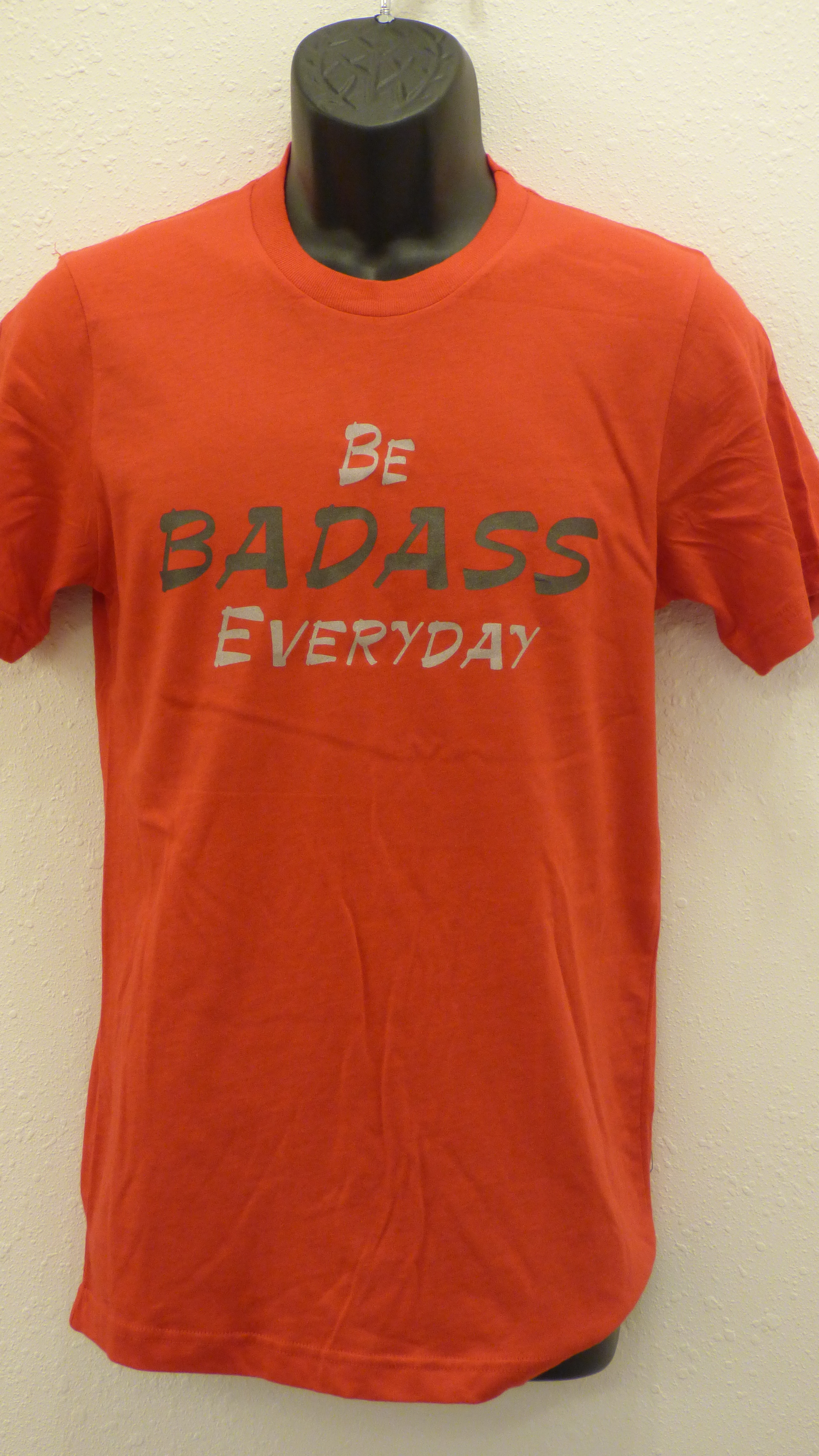
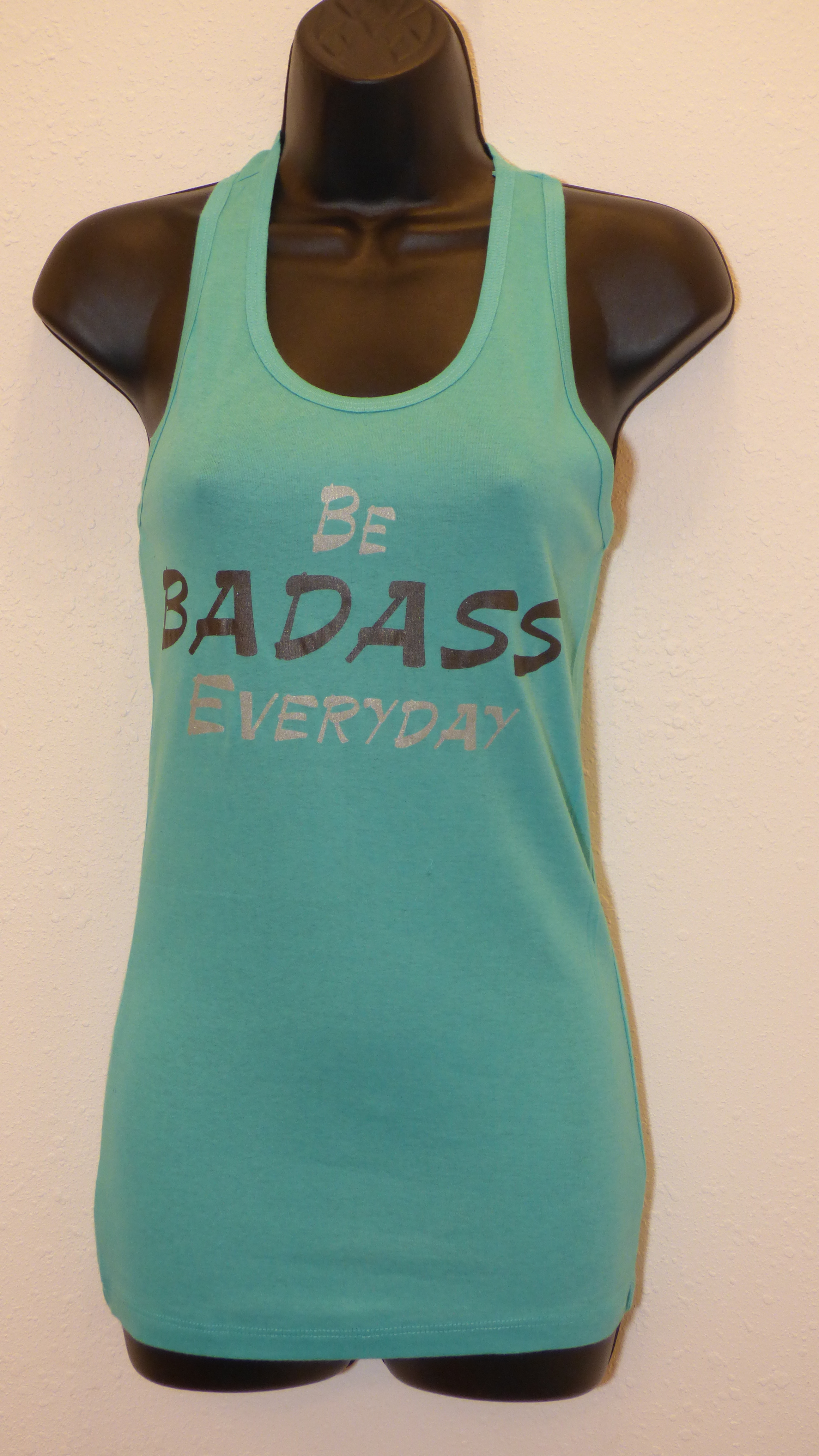
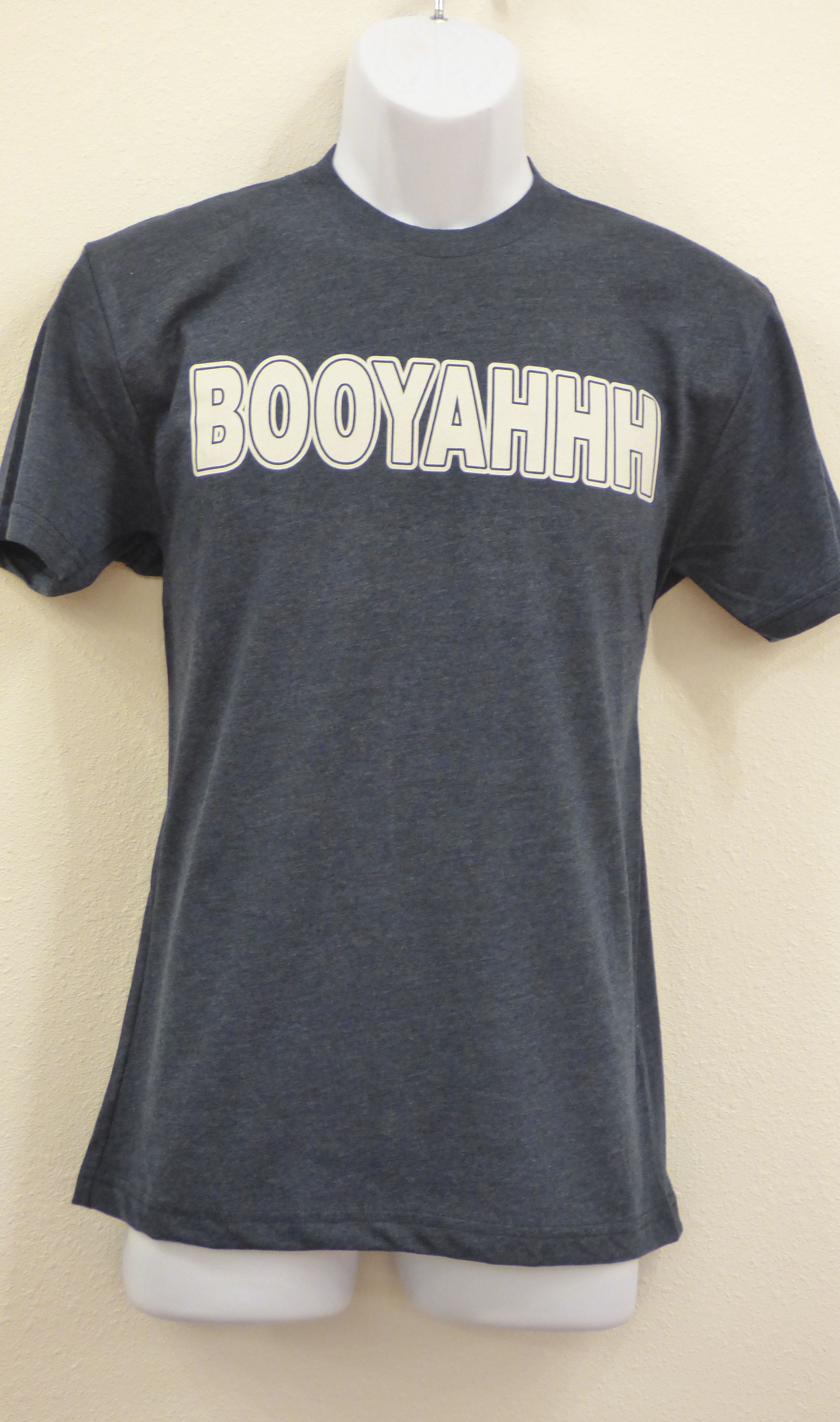
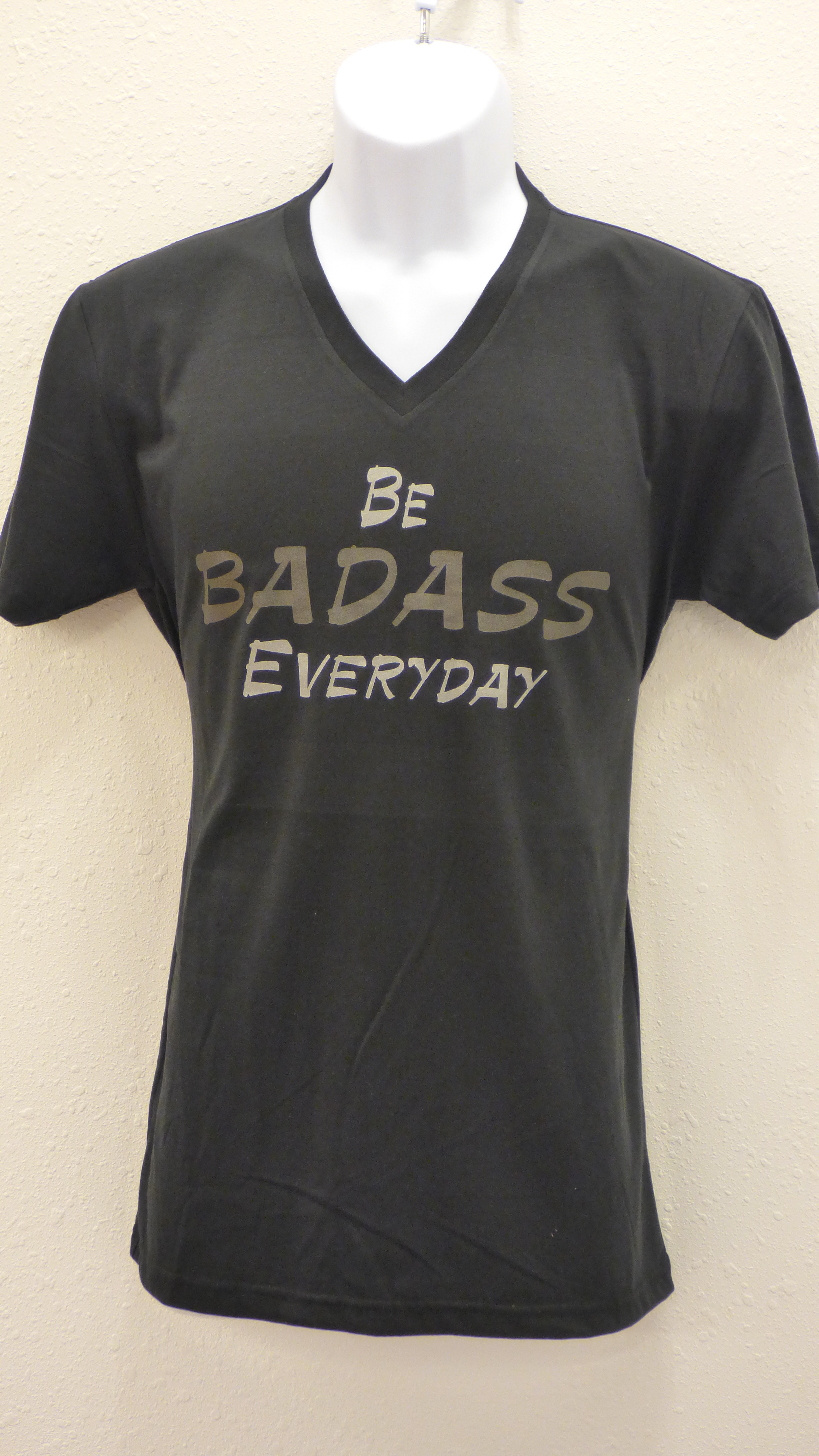
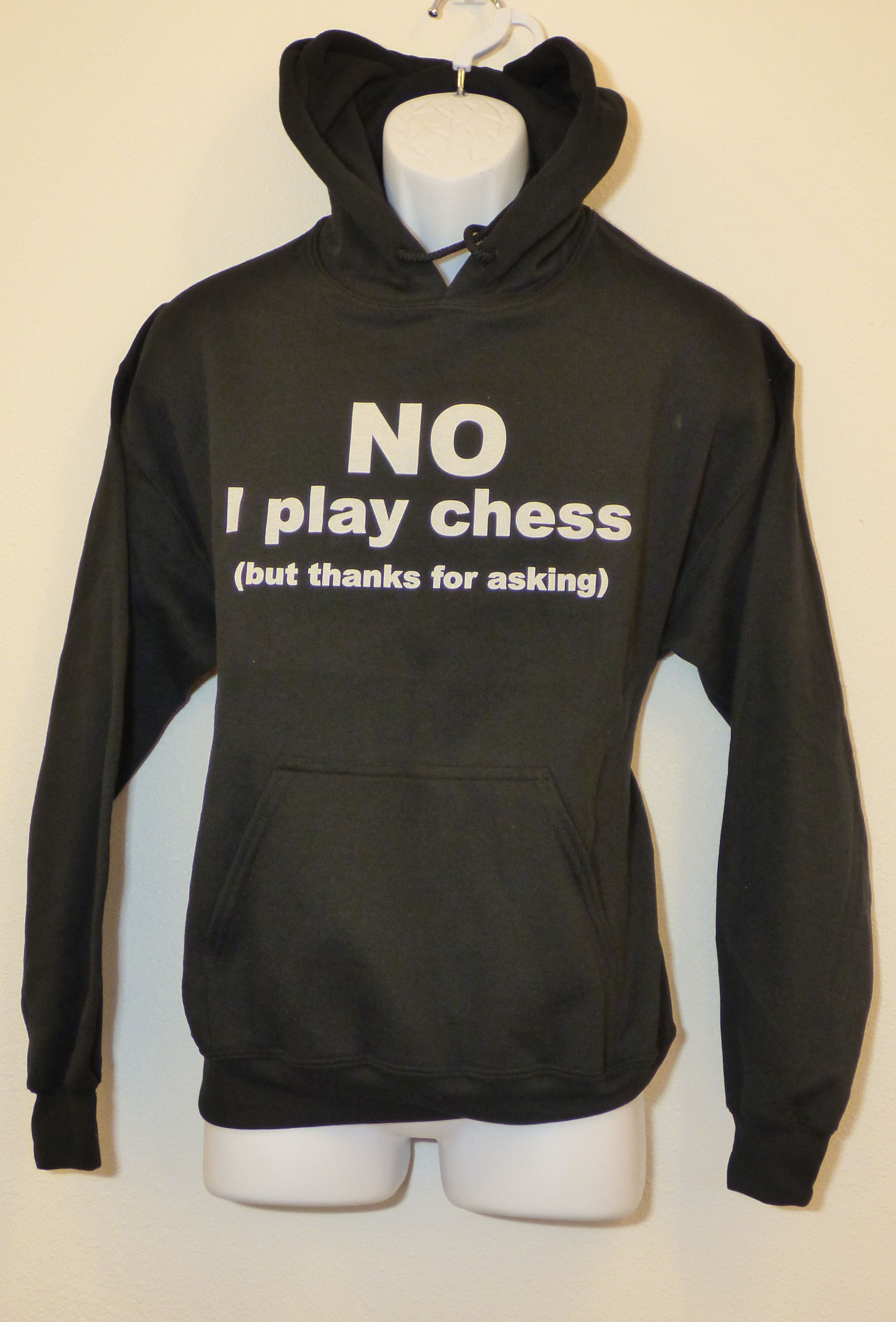
I believe it was July 1st or 2nd that Jeff Kahrs and myself started the latest remodel project here at my home. I wanted to convert the T-shirt business area (about 500+ sq ft) out in my detached garage that also housed the gym into another Traveling Nurses suite, But to do that, we needed to redo the existing bathroom shower, bust through the concrete slab in the shower to tie into the sink that would be going on the other side of the wall, and make a new bathroom for the gym off of the existing one. Jeff tackled the concrete in the shower stall. I tore into the concrete out in the gym where the new toilet would go. I masked up initially but my breathing was so labored that I took it off after a break and never put it back on. I had to chip out a 15″ x 8″ x 6″ deep block of concrete flooring as we couldn’t get a saw into either spot – just not enough room. Dust. Tons of concrete dust. But it got done. The following day I had to go through the footing. More dust. Trenched 10 feet to tie into existing plumbing and that part was done. I noticed that my breathing was becoming a bit more labored but nothing was affecting Jeff. No big deal as I’d punched through two holes AND dug a trench.
Then it was time to hang some sheetrock. More dust, sheetrock dust this time. And finally I had to waterproof the hardi-back boards in the shower using Red Guard, a paint-on product that’s extremely toxic in enclosed spaces. By now you should be thinking, “Wow Dave, that’s a lot going into your lungs!” You’re exactly right. And I suddenly couldn’t breathe right. I had difficulty taking deep breaths and exhaling all the way. And I was getting fatigued. Extremely fatigued to the point where I needed to take a couple of naps each day. Add to that I found that I didn’t have energy to do my usual 30-45 minutes of cardio. So I stopped all cardio about a week into the remodel. And then the weight training had to fall by the wayside. That happened at the end of the 2nd week. I. Was. Exhausted! I finally had to stop working on the remodel. “Jeff, I’m exhausted, dude. I can’t breathe and my lungs are heavy. I’m gonna take the next few days off.”
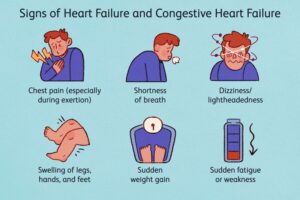
I attributed all of this to the concrete and sheetrock dust, along with the Red Guard toxic fumes in my lungs. “I’ve got some lung inflammation and irritation going on. Lemme rest up a few days and everything will resolve itself and I’ll be fine.” A week goes by. I’m still inflamed. Another week. No better. Finally into the 3rd week of little to no activity (Aug 8th to be exact) I noticed that I wasn’t sleeping like usual. I’d wake up in the middle of the night with a bit of a pounding chest and this deep pressure feeling and inability to breathe. I couldn’t take deep breaths anymore. But dumb ole me kept thinking it was the lungs. Even using “Dr. Google”, I googled my signs and symptoms of lung inflammation and irritation and yup, that’s what I was experiencing. So I “knew” what the problem was. Except I didn’t know.
The next six mornings I’d wake up at 3:30ish am like clockwork with the pounding chest, deep pressure, and inability to breathe. I’d get out of bed, go get a glass of water, and just recline on my living room chair. Somehow I figured out that approximately 45° was the best position to recline to where I could breathe with the least chest/lung pressure. That way I could fall back asleep. I monitored myself to ensure I wasn’t getting worse, but I definitely wasn’t getting any better. Now I was starting to wonder what exactly was wrong with me! It had to be more than lungs, right? But I still had no thought of heart. Couldn’t be the heart!
Another thing I noticed was that whenever I’d eat (it didn’t matter what I ate or when I ate it) I’d immediately get sleepy and have to take a nap or go to bed. I’ll explain more on that later.
About the 1st of August I noticed my ankles swelling. And I also noticed that I was picking up weight…a couple of lbs every day now, but since mid-July I’d slowly been adding bodyweight. As a person with a Master’s Degree in Excercise Physiology and Exercise Science, I ‘knew’ that swollen ankles were a sign of heart issues. I shouldn’t have edema – swelling of the ankles. But I did. And I dismissed it as part of the lungs issue. Perhaps if I would’ve been in ‘Trainer Mode’, i.e., teaching and helping others, I would’ve caught it, but I didn’t. I was locked into the lungs. Every night I took my mid-calf socks off I noticed the swelling – that line of demarcation where the elastic at the top of the socks cuts into the lower leg. Every couple of days it would get deeper and deeper until Friday, Aug. 12th, it was close to 1/2″ deep. Now I was worried. That’s when everything fell apart for me.
I went to bed Saturday night per usual. Woke up at 3:30ish per usual. Except this time I had a sense of impending doom. I couldn’t breathe. I felt like I was suffocating in my own oxygen. I couldn’t take a deep breath in. I couldn’t exhale all the way out. Every breath resulted in coughing. I thought, “Okay, enough of this stupidity. I’m calling the VA at 7:30.” I tried to go back to sleep in my recliner but couldn’t. Imagine getting one good breath and then 8-10 shallow ‘puffs’ of breath over and over and over.
I called the VA here in Tacoma at Gravelly Lake at 7 am. Every 3-4 words I had to pause and attempt to take a breath. Speaking was slow, labored, and deliberate. The nurse on call triaged me. I described what and how I was feeling, and how I’d gotten to this point. She asked, “Mr. Patterson, can you drive to the Seattle VA Emergency Room?” I replied, “Yes, I can do that.” She responded, “Go now.”
30 minutes later I was in the VA emergency room checking in. Within 5 minutes they had whisked me back into one of the bays. An I.V. line was hooked up. A chest x-ray machine was brought in. Ultrasound. An EKG monitor was hooked up. Blood was drawn. More blood was drawn. And then the wait. Finally the ER doctor came in.
“Mr. Patterson, we’re going to give you something to lower your blood pressure. It’s extremely high and your pulse is somewhere between 110-120. Is any of this normal for you?”
“Absolutely not, sir! I’ve always maintained around a 50 pulse for over 30 years and I’ve never had high blood pressure!”
“Well, let’s get you on the medication and get it under control. You should be feeling better in a few minutes. I’ll be back soon.”
The meds do their job. Within 5 minutes I can breathe again albeit with still slightly labored effort, and I can still feel the noisy crepitus in my lungs, which I’m STILL attributing to lung issues. The ER doctor comes back in.
“Well, the good news, is that you don’t have any major lung issues that we could find outside of some fluid on the lungs.”
“So what’s causing all of this,” I ask?
“You have a bad heart. You have severe heart damage, Mr. Patterson.”
After the initial shock of things, my next response was classic me. “So how do we make it better? What can you do? How do we treat this? What do I do? Is this reversible? When you say severe, what exactly are we talking about? Will I need surgery? Can you tell me how long I’ve had this? How come none of this presented before?” I fired off every question I could think of to make sense of this. And then he said, “You’ll get more answers from the cardiologist teams. I’m admitting you to the hospital upstairs.”
Once I got upstairs I was placed in a quad room – a room with 4 veterans. More blood drawn. More imaging. An IV diuretic of 20 mg Lasix was given for the swelling. Questions, questions, and more questions as everyone was trying to figure out how this happened with no warning or markers in my medical jacket. They ended up pulling almost 20 lbs of fluid out of me. I’d topped out prior to going in at close to 190. I typically sit at 170ish. The fourth morning in the hospital I weighed 163. That’s 2 lbs off of my contest weight, but I DIDN’T have a contest look.
I could continue but I think you guys get the gist of everything that went down. I had great nurses and great cardiologist teams treating me. After 3 nights and 4 days in Le Hotel VA, I was discharged with 5 different heart medications. I have to chart my morning and night bodyweight, morning and night blood pressure, and morning and night heart rate/pulse until I physically see my cardiologist in Sept. No big deal on that. I’m used to charting things for this body anyway from the years of bodybuilding and living the fitness lifestyle. The diet they gave me is ‘heart healthy’. I call it the bodybuilding lifestyle diet. It’s pretty much the same things I’ve been eating for years which is how I kept my weight and look under control. So once they were told that, it added to the confusion. The cardiologist teams were like, “Wait…you already eat this way, have been for years, and still this happened?” It just goes to show you that the human body will do what it wants to do when it wants to do it, I suppose.
I want to share with you guys just a little bit on what CHF – Chronic Heart Failure – is and what my cardiologist wrote up. If this blog can help one person seek medical attention, then all of this was worth it.
My cardiologist wrote, “Mr. Patterson, you were hospitalized from 8/13 to 8/17 for shortness of breath and chest pressure. Your echo [cardiogram] (ultrasound of your heart) revealed a new diagnosis of heart failure with a reduced ejection fracture (a measurement, expressed as a percentage, of how much blood the left ventricle pumps out with each contraction – in Exercise Physiology we call this Stroke Volume) of 30-35%. Normal ejection fracture is 60-75%. Your cardiac catheterization (sending two lines into my heart, one from the wrist and one from my neck) reassuringly revealed no coronary artery disease (Congestive Heart Failure or CHF) meaning you had no plaque in the blood vessels to your heart. Tests are still pending that could help better explain your new heart failure diagnosis, but in the meantime we have started you on several meds for your heart function. You were also found to have an arrhythmia called atrial flutter and a clot in the left ventricle of your heart. Your clot is being treated with a blood thinner (Abixiban), and it is very important that you take this consistently to reduce the risk of stroke. Cardiology would like to see you again in 1-2 weeks and then in 4 weeks to repeat an echo. They may also offer you a procedure called cardioversion (aka shock therapy) to treat your atrial flutter. You also had some protein and blood in your urine. Nephrology would like to see you and possibly do a biopsy of your kidney but they would like to wait until your blood clot has been treated for a month (on a positive note, my kidney levels have already improved).”
So what is CHF? Well, basically there are two types of heart failure which are used interchangeably. There’s a left-side heart failure called Congestive Heart Failure and a right-side heart failure called Chronic Heart Failure. I’m not quite sure if I have the right side heart failure OR the left-side heart failure with the reduced ejection fraction. Here’s information on both.
Left-sided heart failure
The heart’s pumping action moves oxygen-rich blood as it travels from the lungs to the left atrium, then on to the left ventricle, which pumps it to the rest of the body. The left ventricle supplies most of the heart’s pumping power, so it’s larger than the other chambers and essential for normal function. In left-sided or left ventricular (LV) heart failure, the left side of the heart must work harder to pump the same amount of blood.
There are two types of left-sided heart failure. Drug treatments are different for the two types.
- Heart failure with reduced ejection fraction (HFrEF), also called systolic failure: The left ventricle loses its ability to contract normally. The heart can’t pump with enough force to push enough blood into circulation.
- Heart failure with preserved ejection fraction (HFpEF), also called diastolic failure (or diastolic dysfunction): The left ventricle loses its ability to relax normally (because the muscle has become stiff). The heart can’t properly fill with blood during the resting period between each beat.
Right-sided heart failure
The heart’s pumping action moves “used” blood that returns to the heart through the veins through the right atrium into the right ventricle. The right ventricle then pumps the blood back out of the heart into the lungs to be replenished with oxygen.
Right-sided or right ventricular (RV) heart failure usually occurs as a result of left-sided failure. When the left ventricle fails, increased fluid pressure is, in effect, transferred back through the lungs, ultimately damaging the heart’s right side. When the right side loses pumping power, blood backs up in the body’s veins. This usually causes swelling or congestion in the legs, ankles and swelling within the abdomen such as the GI tract and liver (causing ascites).
Congestive heart failure
Congestive heart failure (CHF) is a type of heart failure which requires seeking timely medical attention, although sometimes the two terms are used interchangeably as mentioned earlier.
As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the body’s tissues. Often swelling (edema) results. Most often there’s swelling in the legs and ankles, but it can happen in other parts of the body, too. I experienced this.
Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down. This is called pulmonary edema and if left untreated can cause respiratory distress. I experienced this as well.
Heart failure also affects the kidneys’ ability to dispose of sodium and water. This retained water also increases swelling in the body’s tissues (edema). Source: https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/types-of-heart-failure
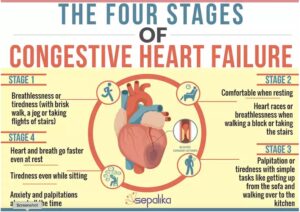
THE FOUR STAGES OF HEART FAILURE
Congestive Heart Failure doesn’t happen in a day; it takes many months if not years to develop. To help stage patients and their treatments correctly, doctors use a four-stage classification of Congestive Heart Failure. Each stage is accompanied by certain mechanisms happening inside the body, but what really matters to us is what we can see outside, as symptoms and therefore, how seriously we need to take them.
The stages of Congestive Heart Failure based on this approach are:
- Stage 1: Normal physical activity like walking or taking a flight of stairs does not lead to shortness of breath, fatigue, or palpitations. However, when you do any moderate exercise, like a brisk walk or a jog or taking four flights of stairs, you feel breathless or tired.
- Stage 2: You feel comfortable when you are resting. But as soon as you take a flight of stairs or walk a block, you may feel breathless or feel your heart race or feel tired.
- Stage 3: You feel okay till you’re at rest. But even the simple task of getting up from the sofa and walking over to the kitchen causes makes you want to rest or pant or feel palpitations.
- Stage 4: You feel your heart and breath faster even at rest, tire even though you are sitting and feel anxiety and palpitations almost all the time.
Congestive Heart Failure: Symptoms
Symptoms of Congestive Heart Failure are divided by doctors based on which side of the heart is affected – the right or the left. However, since both sides of the heart eventually affect the functioning of the other side, it is simpler to look at all the symptoms that could occur with Congestive Heart Failure:
- Shortness of breath upon lying down or physical activity or even at rest, rapid, shallow breathing, cough that is persistent, excess phlegm formation
- Heaviness of heart, fast heart rate, missing beats or arrhythmias
- Swelling In the legs – especially the ankles, in the chest, around the lungs, in the abdomen, around the liver and spleen
- Overall Tiredness, fatigue, muscle pain, loss of appetite, feeling restless, weight gain
- Brain fog, confusion, loss of memory
- Excess urination, especially at night
- Chest pain, abdomen pain and leg pain, with the swelling that puts pressure on these areas. Source: https://www.sepalika.com/heart/congestive-heart-failure/
CHF usually cannot be cured. With treatment, my symptoms will be controlled, and my quality of life will improve. With proper management I’ll feel better and have more energy. In fact, I already am feeling significantly better! I’m back to training in the gym but haven’t started back on the cardio or the projects just yet. Baby step. But rest assured that I’ll get back to everything. This was just a lil’ speedbump in the road of life for me.
If you’ve read this far, you might remember me saying that I’d circle back to explaining the food/fatigue thing. Here’s my thoughts. When you eat, the body shunts blood to the stomach to facilitate the processing and digestion of consumed foods. In a normally functioning heart this is easily done with blood also servicing the brain, meaning no reduced ejection fraction/stroke volume. One doesn’t experience fatigue, and in many instances people notice an increase in energy as carbohydrates are released into the bloodstream providing needed energy and brain fuel. But in my case, because I have the restrictive blood flow coming from the heart, eating took up the less-than-normal amount of blood which left less oxygenated blood to make it to the brain. Almost instant fatigue and sleepiness. After an hour or so I’d be fine. Now I can’t categorically say that’s what happened but It sure sounds like a good theory to me!